
A Closer Look at: The Importance of Denial Management
May 15, 2024
Utilizing robust Pre & Post Edit (PPE) solutions to help your pharmacy maximize prescription claim reimbursements is important to ensure that many claim elements that affect payment are submitted correctly. While optimizing reimbursement is one of the primary reasons pharmacies implement PPE solutions, there are several other benefits such as audit protection and operational efficiency that can also have a major impact on your pharmacy’s bottom line.
Today, we take a closer look at the key area of operational efficiency, which means utilizing the edit program to help improve pharmacy workflow and reduce costs. Specifically, we want to examine how PPE solutions can be leveraged to reduce claim rejection volume. Rejected claims often impede pharmacy workflow, drive up labor costs, and increase patient wait times.
Pharmacy claims contain dozens of data elements that each convey something about that claim to the payor. Ensuring that those data elements are populated correctly is challenging and often payor specific, so claim rejections are typically one of the main challenges that pharmacies contend with in terms of slowing down their workflow. Having to correct data elements and rebill claims takes time and requires well-trained employees, which adds additional staffing costs to your bottom line. DetectRx edits check claim elements before they go to the payor and is able to make corrections automatically or provide staff with specific guidance for making the needed adjustments proactively. These interventions result in a much higher percentage of ‘clean’ claims that are accepted and paid appropriately by the payor without any additional rework at the pharmacy. This reduces labor costs and saves on adjudication click fees, which helps protect your pharmacy’s bottom line.
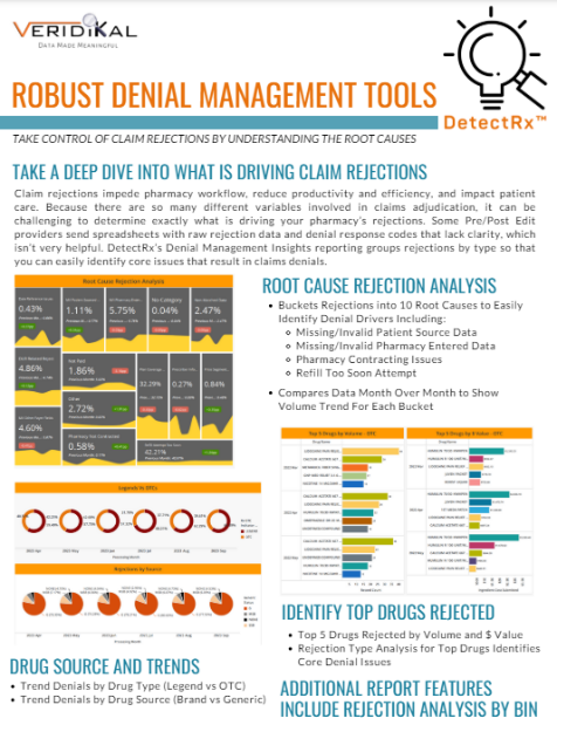
DetectRx provides visually compelling reporting that tells the story of what is driving your pharmacy’s claim rejections. While some Pre/Post edit providers send spreadsheets with raw rejection data and denial response codes, our Denial Management Insights Report provides a detailed rejection analysis that buckets specific rejection reasons so that your pharmacy team can easily determine what the primary rejection types by volume or dollar value. Data is also compared month over month so that you can track changes in reject volume over time. Many of our clients are able to achieve significant reductions in their denied claim volumes by making simple changes that have a big impact.


To learn more about DetectRx, click the Request a Demo button on our website.